California is Seeing an Increase in Mpox Cases. Where Am I Able to Get Vaccinated?

Public health officials are alerting the public to the growing number of cases of mpox, formerly known as monkeypox, throughout California, including the Bay Area, following a summer of unusually low case rates.
The virus first became apparent in the summer and autumn of 2022 in the United States, primarily affecting men who identify as gay or bisexual and transgender or nonbinary who have sex with men. The rate of mpox infections in California nearly disappeared following a large vaccination campaign spearheaded by LGBTQ+ community organisers and public health officials; but, the average number of cases recorded each week throughout the state has more than doubled since the summer.
Read on for information on the recent spike in measles cases in the Bay Area and throughout the state, suggestions from regional public health experts, and locations for the Bay Area measles vaccine.
What is the current condition of mpox cases in the Bay Area and throughout the state?
Much earlier this year, ahead of Pride celebrations in June, Bay Area health officials had been concerned about the possibility of a recurrence of mpox, a virus that mostly transmitted by close physical contact. There was no outbreak similar to the one in 2022, and the number of cases remained extremely low. Data from the California Department of Public Health (CDPH) indicate that, from February to August 2023, the average weekly case count throughout the state of California was between one and seven cases.
Tomás J. Aragón, the director of CDPH, however, declared on October 31 that the organisation was now “beginning to see an uptick in mpox cases across the state.”
From a low this summer to “approximately 17 cases per week in the most recent three-week period,” the number of mpox cases in California has “significantly increased,” according to CDPH data (with available data being from Sept. 20 to Oct. 10).
Additionally, 15 California counties reported mpox cases in the most recent three-week period, up from 11 counties in the three weeks prior, according to CDPH. The government stated that comparable increases are observed across the country in places “such as North Carolina, Hawaii, and Washington.”
The Bay Area, what about it? In August, there were only 7 cases of mpox in the city; by September, there were 20 cases, and by October, there were at least 20 cases, according to a statement from the San Francisco Department of Public Health (SFDPH). SFDPH reported that, although at somewhat different dates from San Francisco’s surge, “some Bay Area counties have seen increased incidence rates in the last several months,” as have other major cities around the country. According to Los Angeles, mpox cases climbed in Chicago in May, while SFDPH saw an increase in mpox cases in June. It was the latter outbreak that first made Bay Area health officials recommend increased watchfulness against mpox in advance of Pride.
How much of a concern is this increase in cases of mpox?
According to CDPH, “mpox continues to circulate in California, and recent data indicate that transmission levels are increasing, even though the average number of weekly cases is still low compared with last year at this time.” Additionally, SFDPH emphasises that the number of cases for October may increase as they continue to count.
Regarding this most recent spike in mpox case counts, CDPH observed two significant developments. The first is that “ongoing transmission within sexual networks” seems to be driving this most recent increase more so than individuals travelling to or from particular locations.
The majority of patients, according to CDPH, “did not report travel or attending any specific event.”
Since transmission of the mpox during this outbreak “is primarily related to intimate contact during oral or anal sex,” and “when people are connecting more frequently or with new sexual partners, there are more opportunities for mpox to spread,” SFDPH has been more receptive to the idea that travel and event attendance may have contributed to this most recent outbreak.
“Events, parties, and travel in the late summer may be linked to changes in sexual behaviour that may result in a rise in cases,” SFDPH stated.
The function of the two-dose mpox vaccine and what it does (and does not) accomplish was the second standout point from CDPH.
According to CPDPH, since early September, more than 40% of individuals with a confirmed case of mpox had received at least one dose of the vaccination. Only 31% of the population received two doses. “While the mpox vaccine is effective at reducing infections and disease severity, infections after vaccination are possible and testing is warranted among vaccinated persons,” the CDPH stated, highlighting this point.
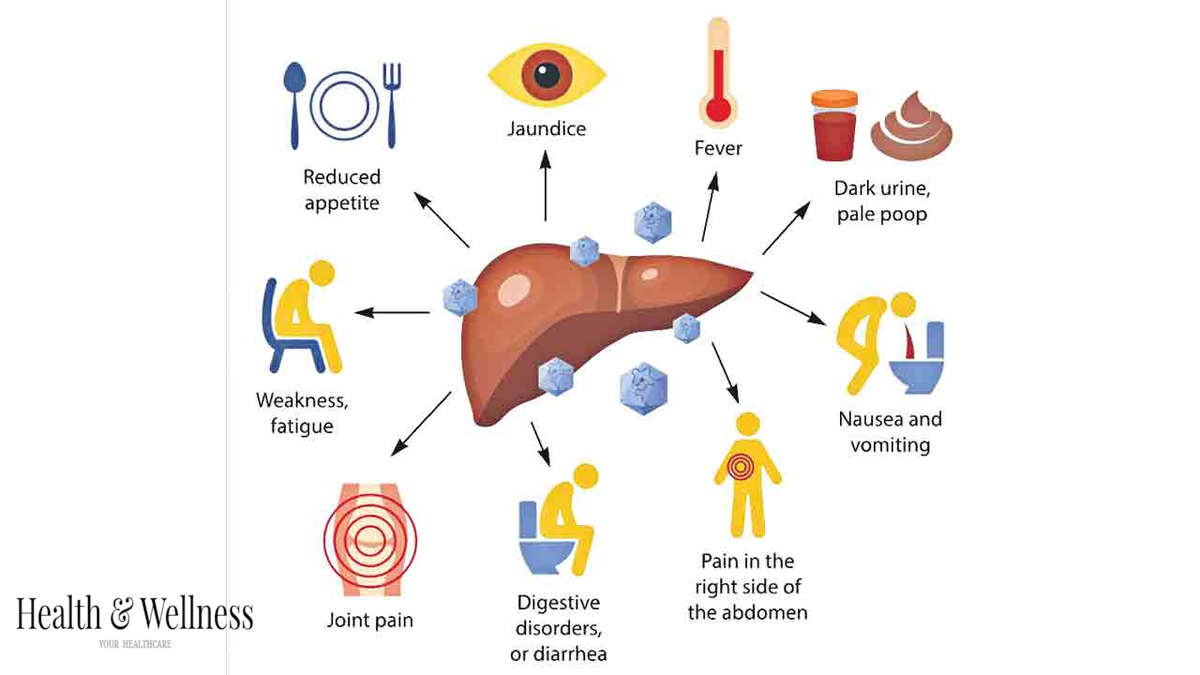
In order to guard against serious sickness, Aragón stated, “with this, we are reminding and encouraging all Californians to be aware of the signs and symptoms of mpox and to take preventive measures, including vaccination.”
The mpox vaccination has been given more than 50,000 times, according to SFDPH, but “more than 40% of those who received their first dose” now need to obtain their second dose. Is there a reason why more people aren’t getting the second dose of the mpox vaccination if case rates are lower in those who have received two injections than in those who have received just one?
The Oakland LGBTQ Community Centre, which provides mpox shots at its clinic, was founded and is led by Joe Hawkins. Hawkins speculated that this summer’s low case rates may have been influenced by the “huge number of people out there who received their first dose and who never came back for the second dose.”
Who is most vulnerable to mpox?
Anybody can contract mpox, but according to SFDPH, the 2022 outbreak primarily impacted populations of males who identify as gay or bisexual, men who have sex with men (MSM), and transgender and nonbinary people who have sex with men.
Dr. Stephanie Cohen, director of HIV prevention for the Population Health Division at SFDPH, told KQED earlier this year that the 2022 outbreak was “unique compared to what had been known about mpox previously.” The reason for this is that, according to her, the virus “really seemed to spread through sexual transmission and [was] associated with sexual activities.” Learn more about the spread of mpox.
“Our national data [from 2022] shows that cis men accounted for nearly 97% of cases in the United States,” Cohen stated. “Cisgender women and children under the age of sixteen had very, very few cases—about 0.08% of all cases.”
Must I receive the mpox vaccination?
In view of the most recent spike in cases, public health experts are advising individuals to get vaccinated against mpox. The vaccine is a two-dose series with a month or so between doses. So …
In 2022, if you received both doses of the mpox vaccine:
You don’t need to receive another mpox vaccination in 2023 because you are entirely up to current. According to Cohen of SFDPH, getting an MPOV booster is not advised at this time.
If in 2022 you were not vaccinated against mpox:
Take your first dose as soon as you can, and then another dose about 28 days later.
If you received the mpox vaccination for the first time only in 2022, or more than 28 days ago:
As soon as you can, take your second dose, advised Cohen. “Receiving both vaccination doses is essential for protection,” the speaker stated.
Reminder: Everyone can receive the mpox vaccine.
At first, in 2022, vaccinations were restricted to individuals who had been exposed to mpox or who were classified as belonging to a particular category that was more susceptible to the disease. These qualifying requirements are no longer in place, and San Francisco and many other Californian locations provide the mpox vaccine to anyone who requests one.
The SFDPH website stated that there is “no need to prove eligibility for the vaccine” and that there is “no shortage of mpox vaccine now.”
Recall that, despite the evidence from the CDPH, receiving the mpox vaccination won’t guarantee that you won’t develop the disease. However, receiving a vaccination could also
“It’s undoubtedly a positive result of the vaccination — as there were some quite serious cases of mpox in unvaccinated individuals last summer,” Cohen stated. Furthermore, we sincerely hope that no one will have to go through the agonising and upsetting symptoms that happened simultaneously.
Where can I get the vaccine against mpox?
You do not require health insurance in order to acquire the 100% free mpox vaccine. Similar to the COVID vaccine, getting the mpox vaccine won’t make you a public figure or have any bearing on any upcoming immigration procedures you could go through. Moreover, getting the vaccine won’t require you to answer questions regarding your immigration status.
For the mpox vaccination, you have two options: make an appointment or visit a walk-in facility.
Is monkeypox and mpox the same thing?
Indeed. The World Health Organisation declared in 2022 that, in light of the “racist and stigmatising language online, in other settings, and in some communities” that it claimed to have observed during the outbreak earlier that year, it would adopt the new, preferred term “mpox” as a synonym for monkeypox.
The virus was initially known by SFDPH as MPX, which you may have also encountered.
Carlos Cabrera-Lomelí of KQED contributed to this article.
Tell us: What other information is needed.
At KQED News, we are aware that finding the solutions to problems pertaining to navigating the Bay Area in 2023 can occasionally be challenging. We’ve released concise, useful explanations and recommendations on COVID, how to handle severe winter weather, and safe ways to use your right to protest.
Tell us, then: What more information do you require? If you ask us, we might be able to provide you with an online or social media response. Your contributions will strengthen our reporting and assist us in selecting stories for both KQED Public Radio and this website.